There has been a sharp rise in cases of the superbug MRSA being contracted outside hospitals across the UK.
Britons have been urged to avoid sharing items such as towels or razors, particularly in gyms and leisure centres where the bacteria has been spreading.
Figures show that 175 people were infected with MRSA in the community between January and March this year – a 47 per cent increase on the 119 cases recorded during the same period in 2019.
At the same time, those contracting MRSA have been getting younger. Nearly a quarter of community-onset cases in 2023–24 were recorded in people under 45, compared with just one in 10 in 2007 to 2008.
The UK Health Security Agency (UKHSA) said it was “too early” to know if this rise represents a lasting change, but it added that infection rates are being closely tracked.
Here, The Independent takes a look at what MRSA is, what the symptoms are, and how to get treated for it:
What is MRSA?
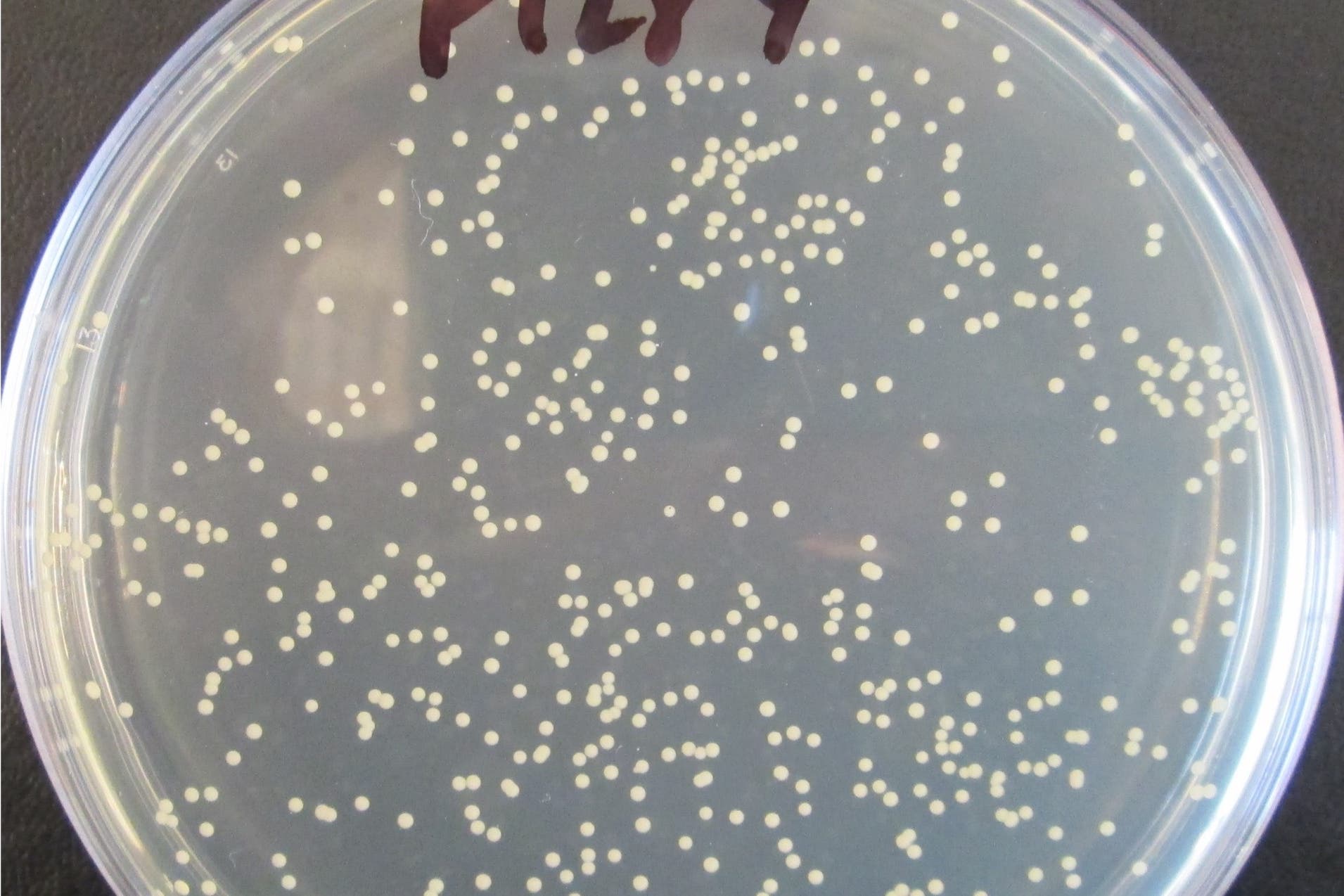
According to the NHS, MRSA (meticillin-resistant Staphylococcus aureus) is a type of bacteria that usually lives harmlessly on the skin.
However, if it gets inside the body, it can cause a serious infection that requires immediate treatment with antibiotics.
The UKHSA explains that Staphylococcus aureus is commonly found on human skin and mucosa (the moist, inner lining of some organs and body cavities). In many cases, it causes no problems.
But when it enters the body, through broken skin or a medical procedure, it can lead to illnesses ranging from infected eczema and abscesses to pneumonia, joint infections, or bloodstream infections.
Most strains of S. aureus can be treated with standard antibiotics, the NHS says, but MRSA is resistant to meticillin and often requires alternative drugs.
What are the symptoms of MRSA?
The NHS says that many people carry MRSA on their skin without showing symptoms. Problems only arise if the bacteria cause an infection.
- According to the NHS, signs of an MRSA skin infection can include:
- Painful, swollen patches of skin
- Warmth in the affected area
- Leaking pus or liquid
- Redness (though this may be harder to spot on brown or black skin)
If MRSA spreads deeper into the body, it can cause more severe symptoms such as:
- High temperature
- Chills
- Dizziness or confusion
- Breathing difficulties
How is MRSA treated?
The treatment of MRSA depends on how serious the infection is.
Mild MRSA infections may be managed with antibiotic tablets, the NHS says.
However, for more severe infections, hospital treatment may be needed. This often involves antibiotics delivered through an injection or a drip. Courses of antibiotics can last from several days to several months, depending on the severity of the infection, according to the NHS.
In cases where abscesses or collections of pus form, surgery may be required to drain the infected area.
How can MRSA be prevented?
The NHS advises that people staying in hospitals or care homes face a higher risk of MRSA, especially if they are undergoing surgery.
Visitors are urged to follow strict hygiene instructions, including washing or sanitising their hands.
The spread outside of hospital and care settings can be reduced through everyday hygiene measures:
- Regular handwashing
- Avoiding sharing towels, razors, or personal items
- Keeping cuts and wounds clean and covered
Before surgery, patients may be offered an MRSA screening test, the NHS says. This involves taking swabs from the nostrils, mouth or groin. If MRSA is detected, a short course of antibacterial cream, shampoo and body wash is usually prescribed to clear the bacteria before the procedure.
Who is most at risk?
The NHS says MRSA can affect anyone, but some people face a higher risk, including those who:
- Spend long periods in hospital for serious conditions
- Have wounds, surgical cuts, burns, or drips inserted into veins
- Have weakened immune systems due to conditions such as HIV or treatments like chemotherapy
The UKHSA warns that while most infections can be treated, resistant strains such as MRSA present more challenges, making prevention and monitoring vital.




