Trans people are increasingly travelling abroad to countries such as Thailand to undergo gender-reassignment surgeries (GRS), with lengthy NHS backlogs resulting in some patients waiting up to 20 years for treatment.
Charities have warned that difficulties in accessing healthcare in the UK harm patients’ mental health and create a “desolate experience” for the trans community.
As a result, there has been a rise in recent years of trans people taking increasingly drastic action by paying thousands to travel to countries such as Thailand, Poland, Spain and Turkey for speedier treatment.
The damning Levy Review, which was published in December, found that waiting times for a first appointment at an NHS adult gender dysphoria clinic are projected to reach 15 years unless there are improvements.
Dr David Levy found that long waiting lists were also driving people to self-source hormone drugs from high-risk online providers abroad, while there was “virtually no other data” available from adult clinics beyond the waiting times.
Freya Firewood, 31, is among several Britons who have travelled to Southeast Asia after she and her partner decided last January to undergo surgery together.
After spending years becoming comfortable in her own body, Freya used her savings to book an appointment abroad, as several of her friends had spent years struggling to access NHS support.
“It feels completely hopeless for some people if they only get placed on the waiting list now,” she said.
Bangkok is a world-leader in GRS and is significantly more cost-effective, with packages often ranging from $9,000-14,000 (£6500-10,000). While there are few private clinics that offer these surgeries in the UK, costs often go beyond £34,000 for vaginoplasty.

While there are no official statistics on the number of people undergoing the surgery in Thailand, it was reported in 2023 that at least 100 Thai doctors are qualified to perform the surgery, and that there are at least 20 medical centres to choose from.
Freya told The Independent: “The appeal is that they have more advanced techniques out there, the price difference, the ability to just book an appointment. For me, I was treated within 9 months.”
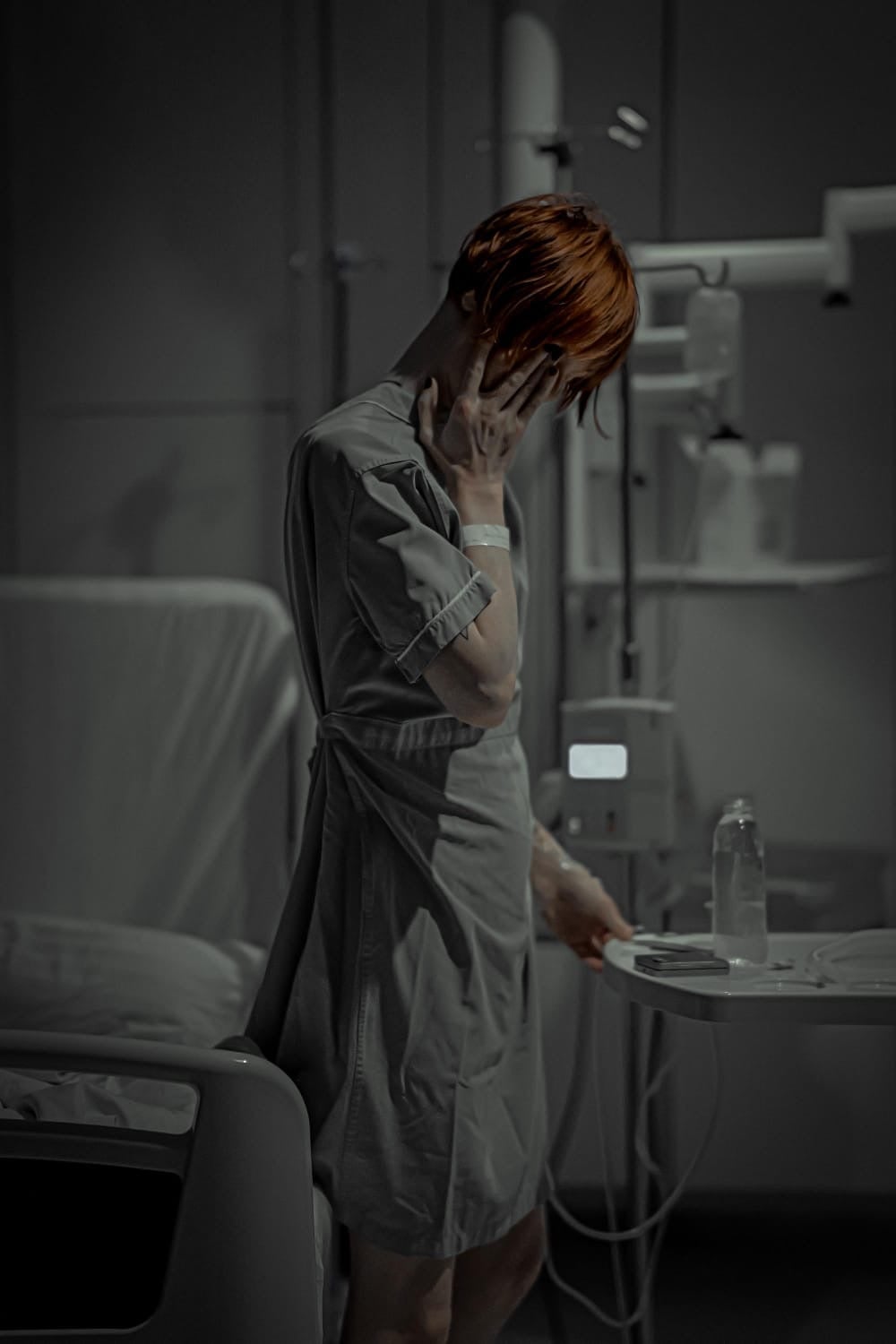
However, while she praised the medical team in Bangkok who have been “amazing”, Freya suffered complications and now faces a difficult six months healing period, before she has to return to Thailand to undergo the same process.
“As soon as we were out of surgery, that was when my problems started,” she said. “I couldn’t urinate, I need a catheter. I then found extra drainage holes either side of my vagina opening up and I couldn’t walk for more than half an hour.”
She added: “It’s something I’ve had to come to terms with, it’s like getting an entirely new body but not entirely the one I asked for.”
As a result, Freya spent two months in a hotel in the city before returning to London, and is now concerned that her surgery complications could impact her career and her finances, given that she will have to fly out again later this year.
She said: “There has been this whole process and it’s never quite worked out. I’ve had this struggle of knowing it hasn’t quite worked out and that has been completely crushing. I’m going to be a woman with no vagina.”
While the vast majority have positive treatment experiences abroad, charities and organisations have raised concerns that trans people now feel they have no other choice but to travel given how inaccessible treatment is on the NHS.
Alex Matheson, director of inclusion at the charity LGBT, said: “There’s always going to be a risk when you travel for surgery even with the best quality of care, there is an element of risk for surgical intervention.
“You potentially don’t speak the language, you have limited access to services, aside from the ones you’ve paid for, there are the risks to mental health. Even with the best possible outcomes, you’re going through a treatment that is invasive, and bound by your emotions, and you’re potentially doing it without your support network.”
While the NHS will treat life-threatening, emergency complications from surgeries abroad, they are not obligated to provide routine, follow-up, or corrective surgery for procedures privately funded outside the UK.
As a result, Freya will maintain regular contact with a group of professionals in Thailand, and is crowdfunding to help finance her return trip.
Referring to the waiting list, Ms Matheson said: “In all honesty, it’s a desolate experience for a lot of people. We are seeing poor outcomes across the board for trans people who are waiting. It could be five to seven years for your first appointment, or 10 years for a diagnosis to receive gender affirming surgery. Somebody could potentially go through 20 years of waiting before getting to the point Freya is at after surgery – that’s quite horrific when you think of the impact that has on someone.”
Published in 2024, the Cass Review, which looked at gender identity services for under-18s, called on gender services to match the standards of other NHS care.
It came after concerns were raised about the Gender Identity and Development Service (Gids) at the Tavistock Centre, which was the only specialist clinic for young people, and was closed shortly before the review.
In the Levy Review, it was noted that a significant portion of referrals came from those who had aged out of youth services.
Tammy Hymas, a policy lead at the advocacy group TransActual, said: “A survey found overwhelming evidence that these long waits were really impacting on mental health.
“We know there have been several cases lately, and coroner reports, that sometimes people have taken their own lives. It’s a national scandal and it is a crisis we’re experiencing. The NHS is not stepping up to the scale of the crisis.”
She continued: “It drives people to other options and those do include going abroad, to Thailand, Spain and Poland. It’s absolutely an increasingly common phenomenon. It’s a huge social justice issue because only those who can afford it can actually do it, it’s a bit of a trans tax. Trans people will spend thousands of extra pounds a year on gender affirming care and that’s money a lot of people don’t have in a cost of living crisis.
“It’s a difficult situation for a lot of people as the impact of waiting is really dangerous for people’s mental health.”
NHS England have been approached for comment.


