The Mpox patient that sticks most clearly in Dr Elin Hoffman Dahl’s mind had lesions all over his body: in his mouth making it agony to eat; painful swellings under his feet meaning even walking to the toilet was a struggle, while the skin was “almost completely gone” from a number of other areas.
“He was a very beautiful person and I remember he asked for a small mirror. It was very heartbreaking to see,” Dr Hoffman Dahl says.
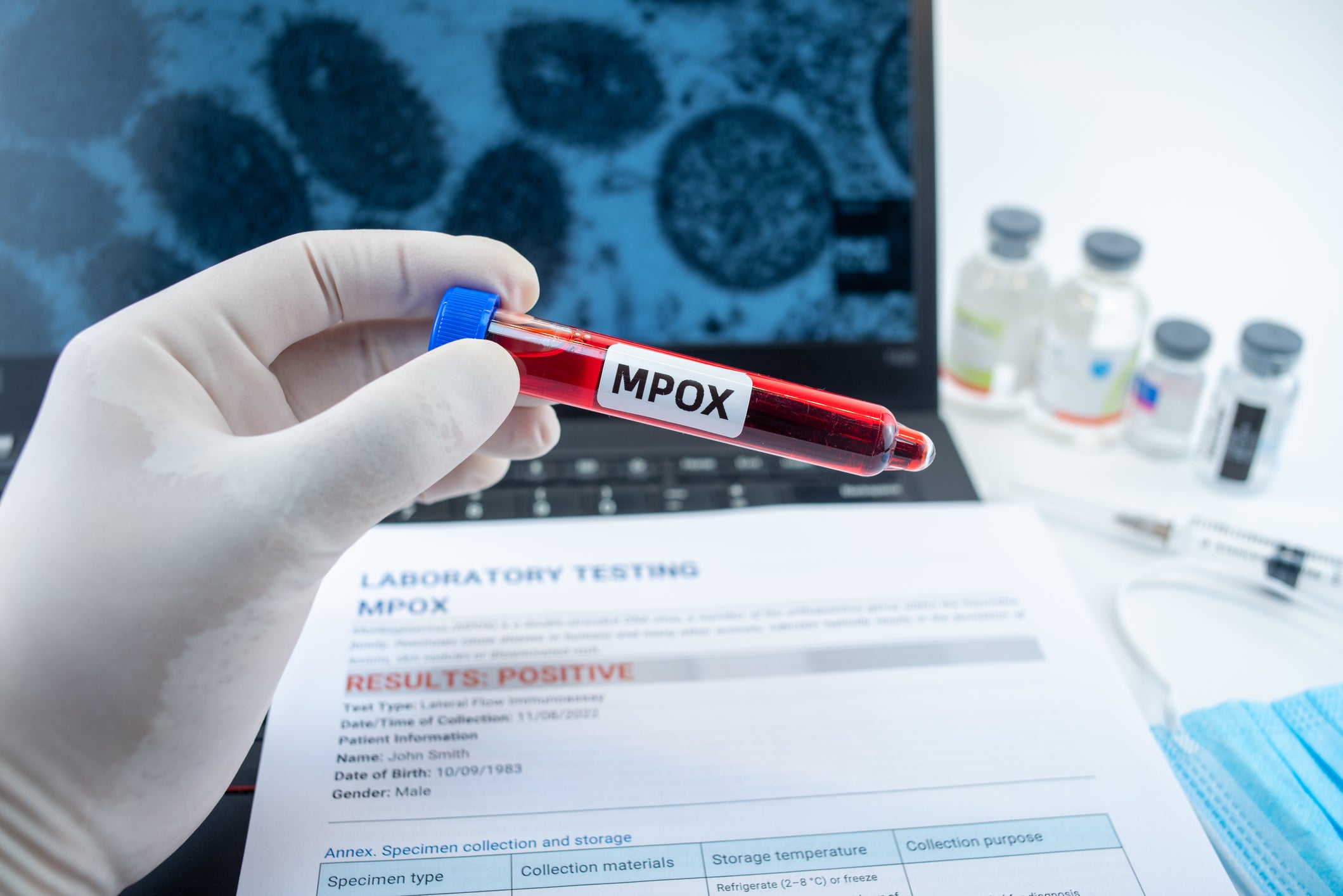
For many people, Mpox is a relatively mild though uncomfortable virus that clears up without specific treatment. But in Sierra Leone, where Dr Hoffman Dahl was deployed to support the country’s outbreak with Medecins Sans Frontieres (MSF), an epidemic of untreated HIV has transformed it into a deadly disease for some.
While Sierra Leone’s outbreak response is largely being heralded as a success story, Mpox has revealed that the scale of HIV in the country may be far higher than national data suggests. Meanwhile, Trump’s aid cuts left the country scrambling to plug gaps in programmes that has likely hampered the speed of its response, activists have told The Independent.
The first Mpox cases were recorded in January this year and from April they began to spike. Dr Hoffman Dahl, an infectious diseases doctor in Norway, travelled with MSF to join a team of highly-skilled Sierra Leonean doctors – well-accustomed to dealing with infectious-disease outbreaks. But she and her team were alarmed by the rates of HIV they were finding in their Mpox patients, several times higher than the estimated national average of 1.7 per cent.
Dr Hoffman Dahl says this was a surprise in a country that’s considered to have a relatively low HIV burden. Her colleagues who had worked on Mpox in Democratic Republic of Congo were taken aback by the severity of the skin damage they were seeing.

As well as cases of undiagnosed HIV, “I think one striking thing was that there was also quite a high number of people who had been diagnosed previously, but were not on treatment. And that, of course, tells you something – that it’s a stigma to be on treatment,” Dr Hoffman Dahl says. I had, for example, one patient who I was very open about [having]… stopped his medication two years ago.”
With medication, people living with HIV can generally deal with infections like anyone without the virus. But when Mpox finds someone with untreated HIV, whose immune system is severely compromised, it becomes a different story.
Then, the aim becomes, “to start people on HIV medicines and keep them alive until their immune system is able to heal the skin,” Dr Hoffman Dahl explains: “to keep them alive long enough for the medicines to reconstruct the immune system and to bring down the HIV virus.”
For her patient, this proved impossible.
‘Covering the gap’
“We managed to get [his] daughter to see him,” she recalls – he hadn’t seen her for months, reluctant to be seen so sick. “Two or three days later he died,” Dr Hoffman Dahl says, of complications from the infections battling it out in his body.
“It’s quite devastating…as a doctor you understand where it’s going and you feel like you’re not able to do enough”. Without enough labs, the more expensive antibiotics needed to deal with resistant infections and experimental anti-virals for Mpox that might be available in richer countries: “You’re not able to keep him alive just long enough for the drugs to be working.”
James Riak Mathiang, health programme manager for humanitarian charity GOAL Sierra Leone, worked closely with the country’s National Public Health Agency when Mpox cases emerged, to raise public awareness and work with communities to prevent more cases.
But the higher burden of HIV won’t be focused on until Mpox cases have been brought to zero, he says. Only after that will there be “further questions”, despite the fact that for some, their Mpox will never be brought under control unless their HIV is treated.
The impact on the Mpox response of Trump’s slashing foreign assistance spending down to the bare bones has been huge according to Riak Mathiang.
The biggest effect is from the loss of what’s known as flexible funding from the now-shuttered US Agency for International Development (USAID), he thinks. That’s money not earmarked for a specific programme, giving outbreak management teams the leeway to respond “immediately”.
“Let’s say there’s an outbreak today; tomorrow you can start the response,” Riak Mathiang says, including testing and paying for health workers and hospital beds.
“Even the partners who may not been affected by USAID directly, they have to reposition or repurpose their budget to cover the gap,” he says, leaching from other sources of ready money. As a result, not as many organisations came on board to support the response as they had during Covid or past Ebola outbreaks.
The cuts could have another, longer-term effect too. Where they hit programmes for HIV and TB, they risk driving up those infections which creates more immune-compromised people for Mpox to attack, Dr Mohamed Bella Jalloh explains .
“Those funding cuts can have an effect on the outbreak because the people most affected by those funding cuts are the ones also likely most affected by Mpox,” says Dr Jalloh, a doctor from Sierra Leone currently conducting research in Canada.
Sierra Leone’s outbreak response has become a model for other countries in Africa, Riak Mathiang explains. Despite global shortages of Mpox vaccines, the country has managed to get more than 200,000 doses into the country.
“Case management, surveillance, even risk communication at urban areas, is also going very well,” he says while the government was able to add 400 beds to quarantine Mpox cases in hospitals.
Where the response fell short, he thinks, was in its slow start and delays in getting traditional leaders in rural areas on board.
Jedidah Johnson is a doctor working in the private sector who found herself unable to get a vaccine, despite treating patients with Mpox symptoms. She contracted the virus herself, having to isolate from her two small children and developing lesions on her eyes. She understood that government health workers were being prioritised, but became “very frustrated” when she began to hear of others who were getting the vaccine ahead of her and her colleagues – seemingly because of personal connections.
“These were people who were not health care workers. They were not immunocompromised or high risk in any way. But they were able to get the vaccine and I was not because I work in the private sector but I am a frontline healthcare worker and I was seeing patients that were meeting the definition for Mpox,” Dr Johnson says.
Her concerns were not just for herself but for unvaccinated HIV patients who were the most affected.
“I think HIV is a much bigger problem than we let on because you know so many people…present with very late disease and so many people are in denial and are not taking treatment,” she says.
Dropping cases
Though the situation is a completely different one to what it was in early summer, Sierra Leone is still working towards zero cases – and as much as it is not the first, this is guaranteed not to be the last outbreak the country sees.
“I recall I was sitting in medical school during the Ebola outbreak and so we had a lot of foreign experts in, you know managing things…but less so during this current Mpox outbreak,” says Dr Jalloh.
This could be a sign of the dwindling global support for foreign assistance, but there is a brighter side too, he thinks.
He can see more local leadership in managing the response to this outbreak and a “more African-led” operation.
“And in the past couple of weeks, you’ve seen [a] 50 per cent drop in the cases”.
Ambitions to move away from aid dependency are nothing new and national agencies to take on responsibility were already taking shape, but cuts from major donor countries may have forced the issue.
“These conversations had been going on for a long time but even when you’re having conversations, you’re dragging your feet,” Dr Jalloh says, whereas the “shocks” of aid cuts from the US and others have been a “wake-up call. Let’s get things going, right”.
“Aid should not define your agenda”.
This article was produced as part of The Independent’s Rethinking Global Aid project




