Groundbreaking artificial intelligence tools, developed by a researcher at a Scottish university, are set to revolutionise skin cancer diagnosis, offering rapid and potentially life-saving assessments to individuals in the world’s most remote regions.
Tess Watt, a PhD student at Heriot-Watt University in Edinburgh, spearheaded the project, envisioning a future where early detection of skin conditions is accessible globally, without direct access to dermatologists or internet.
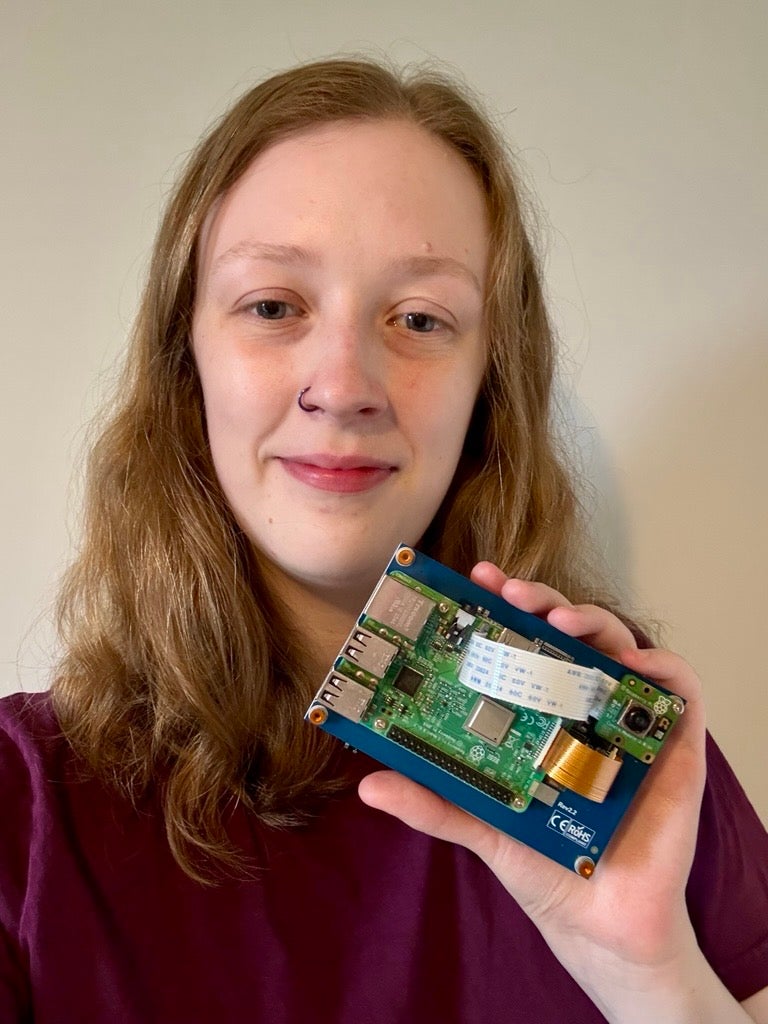
The system involves a patient taking a photograph of their skin complaint using a small camera attached to a Raspberry Pi device – an inexpensive, energy-efficient handheld computer.
This device stores an enormous dataset of thousands of images, against which the photograph is analysed in real-time using state-of-the-art image classification to reach a diagnosis.
These findings are then promptly shared with a local GP service, enabling the initiation of an appropriate treatment plan.
The project is understood to be the first of its kind to combine AI medical diagnosis with the aim of serving remote communities.
Ms Watt explained: “Healthcare from home is a really important topic at the moment, especially as GP wait times continue to grow.
“If we can empower people to monitor skin conditions from their own homes using AI, we can dramatically reduce delays in diagnosis.”
A prototype of the device has already been demonstrated at Heriot-Watt’s advanced health and care technologies suite.
The research team said the tool is up to 85 per cent accurate in its diagnostic capabilities, but they hope to increase this further by gaining access to more skin lesion datasets, aided by advanced machine tools.
Ms Watt is also in talks with NHS Scotland to begin the ethical approval process for testing the technology in real-world clinical settings.
“Hopefully in the next year or two, we’ll have a pilot project under way,” she said, noting medical technology often takes years to move from prototype to implementation.
She added: “By the time I finish my PhD, three years from now, I’d love to see something well into the pipeline that’s on its way to real-world use.”
The university said the long-term vision is to roll the system out first across remote regions of Scotland, before expanding to global areas with limited access to dermatological care.
It added the technology could also offer vital support to patients who are infirm or unable to travel, allowing loved ones to assist with capturing and submitting diagnostic images to GPs.
Ms Watt’s academic supervisor, Dr Christos Chrysoulas, said: “E-health devices must be engineered to operate independently of external connectivity to ensure continuity of patient service and safety.
“In the event of a network or cloud service failure, such devices must fail safely and maintain all essential clinical operations without functional degradation.
“While auxiliary or non-critical features may become temporarily unavailable, the core diagnostic and even therapeutic capabilities must remain fully operational, in compliance of course with safety and regulatory requirements.
“Ensuring this level of resilience in affordable, low-cost medical devices is the essence of our research, particularly for deployment in resource-limited settings and areas with limited or no connectivity, where uninterrupted patient care must still be guaranteed.”



